The Saskatchewan Science Centre Online! Check out our hilarious and educational web series “SSCTV”, find downloadable resources, explore other cool science links, and tune into the live BUBOCam!
What Is A Vaccine?
Everyone's talking about vaccines, and the information can be confusing. Let's get back to basics for a moment: What is a vaccine?
This article is part of a series explaining the COVID-19 pandemic. Please consider starting at Part 1: What is a virus or check out the whole series by clicking the button below.
What Is A Vaccine?
The first vaccine was used in 1796 when Edward Jenner inoculated an 8-year-old boy with material taken from a cowpox sore on another person, under the hypothesis that having cowpox, which typically has very mild symptoms in humans, would protect against smallpox. Jenner later variolated the boy with smallpox material to test the boy’s reaction: he remained healthy. (HistoryofVaccines.org). As word began to spread about these results it grew in popularity, eventually leading to mass adoption. In fact, the very word, vaccination, is derived from Jenner’s experiment. Vacca is the Latin word for cow. (Science)
Some Terminology
Variolate - As early as 1000CE in Asia, variolation was used as a measure to try and prevent people from dying of smallpox. Variolation is the process of deliberately infecting someone with a controlled dose of smallpox such as dried scabs from smallpox sores.
Innoculate - To implant a microorganism into an environment. In medicine, it typically refers to vaccinations to prevent disease, but in general microbiology, it can be used more generally.
Vaccinate - To innoculate with the specific intent of preventing disease
Immunize - To make someone immune to a disease, to prevent them from getting a disease.
Sources:
National Library of Medicine - Smallpox: A Great And Terrible Scourge
Dictionary.com - “Vaccinate” vs. “Inoculate” vs. “Immunize”: What Are The Differences?
Since then, vaccines have been used as a medical technology to control and, in some cases, eradicate harmful pathogens. As we previously mentioned in our Understanding COVID-19 series, a pathogen is an organism such as “a bacterium, virus, parasite or fungus that can cause disease within the body”
Unlike medicines such as antibiotics, which are usually prescribed once a person has become infected with a pathogen to cure or ease the symptoms of a disease, vaccines work with our natural immune system and responses to prevent becoming infected in the first place, or to reduce the severity of an illness for which you have been inoculated (Immunize BC – What are vaccines?).
“Vaccines train your immune system to create antibodies, just as it does when it’s exposed to a disease. However, because vaccines contain only killed or weakened forms of germs like viruses or bacteria, they do not cause the disease or put you at risk of its complications.”
-World Health Organization
Most, but not all, vaccines introduce weakened or deactivated versions of a pathogen, called antigens, to your immune system through injection, or oral consumption (World Health Organization – Vaccines and Immunization). Once the antigens are introduced, our immune system begins to develop antibodies for that specific antigen, which then combat the pathogen spreading throughout and infecting the body. Our immune system also remembers the antibodies it produces for specific antigens to protect against the same harmful pathogens in the future. This process of developing antibodies and remembering them is called immunization or becoming immune to that pathogen (IMMUNIZE BC – How Do Vaccines Work).
Side Effects
Because vaccines use damaged or inactivated versions of the pathogen, they are very safe, although there can be side effects. Many people feel some muscle discomfort where they received the vaccine if injected, or a few side effects, this is called an inflammatory reaction. These reactions mean your immune system is hard at work doing its job developing the antibodies to fight the pathogen you were vaccinated for. Common side effects may include muscle aches, fever, chills, or headaches (Government of Canada – Vaccine safety, concerns, and possible side effects).
“It is much safer to get the vaccine than to get the disease it prevents.”
-IMMUNIZE BC
Effectiveness of Vaccines
In the late 18th century, smallpox was a pervasive disease. “On average, 3 out of 10 people infected died of from the disease” (Center for Disease Control - History of Small Pox), while those who survived were left with severe scarring of the skin.
Over time, Jenner’s work inspired others to improve upon the original smallpox vaccine and develop vaccines for additional pathogens such as rabies, diphtheria, measles, polio, and many other diseases, including COVID-19.
On May 8, 1980, 196 years after Jenner inoculated the 8-year-old boy, the WHO declared smallpox eradicated from the planet. (CDC: History of Smallpox)
“We now have vaccines to prevent more than 20 life-threatening diseases, helping people of all ages live longer, healthier lives. Immunization currently prevents 2-3 million deaths every year from diseases like diphtheria, tetanus, pertussis, influenza, and measles.”
-World Health Organization
Immunization And Herd Immunity
Vaccinations protect us as individuals against harmful pathogens, but they also help protect others in our communities. Once you become immune to a pathogen by being vaccinated, your chances of spreading the virus are reduced or eliminated.
When enough people become vaccinated against a pathogen in a community, others who cannot be vaccinated are protected, creating an effect called herd immunity, or population immunity. On a basic level, when enough people in a community are vaccinated, pathogens have a difficult time finding a suitable host to replicate in, because the majority of people the pathogen encounters are immune.
When a vaccine becomes available, it is important for as many people to become vaccinated as possible. This is because there are some vulnerable people in our communities that cannot be vaccinated due to underlying health conditions, allergies to vaccine components, or because they do not have access to a vaccine. For example, as of this writing (April 9, 2021), there are no COVID-19 vaccines approved for use in children under the age of 16, though clinical trials are underway.
Watch this brief graphic animation from Harvard Medical School to see how herd immunity works.
Dr. Kara Loos, a genomics research associate from the Institute for Microbial Systems and Society (MISS) at the University of Regina, says that different pathogens require different percentages of herd immunity. For example, Measles is one of the most contagious pathogens on Earth. According to the World Health Organization, it is estimated that 95% of a community needs to be vaccinated against measles to create the required herd immunity to protect the remaining 5% of the population who cannot be vaccinated. By comparison, herd immunity for the polio disease is achieved when about 80% of the population is vaccinated (World Health Organization – Herd Immunity, Lockdowns and COVID-19).
At the beginning of the COVID-19 pandemic, some countries felt that the best way to deal with the disease was through natural herd immunity (Reuters). In all cases, this proved to be disastrous as hundreds of thousands of people died, often overwhelming available health resources. Herd immunity for COVID-19 must be achieved through vaccination. “The proportion of the population that must be vaccinated against COVID-19 to begin inducing herd immunity is not known. This is an important area of research and will likely vary according to the community, the vaccine, the populations prioritized for vaccination, and other factors” (World Health Organization).
An upcoming article will focus specifically on COVID-19 vaccines, and on the different types of vaccines available in the fight against COVID-19. However, this much is clear: the best vaccine for you is the one available to you right now.
Did you find this helpful? Consider making a donation to the Saskatchewan Science Centre!
The COVID-19 Vaccine(s)
This article is part of a series explaining the COVID-19 pandemic. Please consider starting at Part 1: What is a virus or check out the whole series by clicking the button below.
The different COVID-19 vaccines available in the world represent a tremendous success by science. These vaccines were developed, tested, and proven safe very quickly, saving millions of lives around the world.
These vaccines were so successful, in fact, that some people questioned their safety or are/were hesitant to take the vaccine because they thought that it may have been rushed.
The truth is, scientists from all over the world worked on finding vaccines for COVID-19. The seemingly rapid development of the vaccines was not due to corner-cutting or shortcuts but was due to the immense worldwide funding, focus, and collaboration as a result of the severity of the pandemic.
All of the vaccines which have been approved around the world are safe and effective against preventing serious hospitalization and death from COVID-19. In all cases, the small risk of side effects from the vaccines far outweighs the potential risks of contracting COVID-19.
The best vaccine for you is the one that has been approved and which you have access to.
Vaccines that have been approved in different countries around the world include:
Sinovac-CoronaVac - developed by Beijing-based Sinovac. CoronaVac uses inactivated virus toexpose the bodies immune system to the virus without risking serious disease. (https://www.who.int/news/item/01-06-2021-who-validates-sinovac-covid-19-vaccine-for-emergency-use-and-issues-interim-policy-recommendations)
Sputnik V - Developed in Russia, the Sputnik V COVID-19 Vaccine uses a recombinant adenovirus approach. Each of the two doses uses a different adenovirus as vectors (AD26 and Ad5) as vectors to overcome any pre-existing adenovirus immunity in the population. (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00191-4/fulltext)
Pfizer/BioNTech (Comirnaty) - This is an mRNA vaccine. This vaccine uses mRNA to teach our body how to create a protein that triggers an immune response inside our bodies. Our bodies produce the protein, and also produces the antibodies that protect us from those antibodies. mRNA vaccines do not change our DNA and the cells which produce the protein break down once the protein is complete. (https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/pfizer-biontech.html)
Moderna (Spikevax) - Like the Pfizer BioNTech vaccine, this is also an mRNA vaccine. mRNA vaccines teach our cells how to make a protein that will trigger an immune response without using the live virus that causes COVID-19. Once triggered, our body then makes antibodies. These antibodies help us fight the infection if the real virus does enter our body in the future. (https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/moderna.html)
Astra-Zeneca/COVISHIELD (Vaxzevria) - Sometimes known as the Oxford Vaccine, this vaccine uses a harmless virus (the adenovirus) as a delivery system. This adenovirus is not the virus that causes COVID-19; you can not get COVID-19 from this vaccine. There are many different types of adenoviruses, including some that cause colds in humans and that infect other species. Scientists have been using these viruses for decades to deliver the instructions for proteins. (https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/astrazeneca.html)
Johnson & Johnson (Janssen COVID-19 Vaccine) - The active ingredient of COVID-19 Vaccine Janssen, also known as Ad26.COV2-S (recombinant), is a recombinant adenoviral vector that contains the sequence that encodes the spike protein (S) of the SARS-CoV-2 virus. This vaccine was approved with a single dose with no booster required. (https://www.who.int/news/item/12-03-2021-who-adds-janssen-vaccine-to-list-of-safe-and-effective-emergency-tools-against-covid-19)
Click Here For A List Of All Vaccines Approved For Use In Canada
Failed Vaccines
With the large number of successful vaccines which have been deployed around the world and the speed with which they were deployed, some people may have felt that developing a vaccine was easy. This isn’t true; these vaccines were developed quickly due to the billions of dollars of research money, time, collaboration, and effort that was put into developing the vaccines. Hearing about the successful vaccines is an example of Survivorship Bias - a type of cognitive bias that makes us forget about the base rate of failures and instead focus on the relatively small number of successes (https://fs.blog/2019/12/survivorship-bias/).
In fact, some of the world’s largest and most well-known vaccine makers were unable to develop or chose not to develop COVID-19 vaccines, including GlaxoSmithKline, Merck, and Sanofi (https://www.ft.com/content/657b123a-78ba-4fba-b18e-23c07e313331). Australia had been working on their own COVID-19 vaccine at the University of Queensland using a ‘molecular clamp’ approach. The development of this vaccine, which showed promise in early testing, was also halted (https://www.sciencemag.org/news/2020/12/development-unique-australian-covid-19-vaccine-halted).
The bottom line: you can feel safe knowing that when a vaccine is approved for use that it has been thoroughly tested and is safe.
COVID-19 Vaccine Conspiracy Theories
It’s not hard to discover conspiracy theories about almost anything on the internet, COVID-19 vaccines included. From microchips to infertility, misinformation about these life-saving vaccines abounds on the internet.
Sometimes conspiracy theories begin as a joke, other times there is a motive - because the originator wants to make a name or money for themselves or a movement, for example.
Why do people come to believe in conspiracy theories? There are many reasons, but they often stem from a need to explain, accept, or rationalize a discrepancy between what one believes and what one experiences. They can make one feel safe when overwhelmed in the world - like you have it all figured out.
In the case of COVID-19 vaccines, those conspiracy theories can cost lives - the lives of the people who believe in them, and the people around them. It is important to think critically and rely on the advice of established health organizations such as the World Health Organization, Health Canada, and the US Center for Disease Control.
Additional Resources:
WHO COVID-19 Dashboard - https://covid19.who.int/
COVID-19 Vaccines Side Effects - https://www.who.int/news-room/feature-stories/detail/side-effects-of-covid-19-vaccines
COVID-19 Vaccines in Canada - https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/vaccines.html
Understanding MRNA - https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html
Understanding Viral Vector-Based Vaccines - https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/type-viral-vector.html
Government of Saskatchewan COVID-19 Info Page - https://www.saskatchewan.ca/coronavirus
Did you find this article helpful? Donate to the Saskatchewan Science Centre today!
Dr. Kara Loos Shares Her Knowledge About COVID-19
Dr. Kara Loos is a genomics research associate from the Institute for Microbial Systems and Society (MISS) at the University of Regina. In this interview, Dr. Loos answered some of the most frequently asked questions about viruses in general, corona viruses, COVID-19 pandemic, and the future of research in microbiology.
This interview is part of a series explaining the COVID-19 pandemic. Please consider starting at Part 1: What is a virus or check out the whole series by clicking the button below.
About Dr. Kara Loos
Dr. Kara Loos is a genomics research associate from the Institute for Microbial Systems and Society (MISS) at the University of Regina. She has been a part of the team conducting research and testing on SARS-CoV-2.
About the Interview
In this interview, Dr. Kara Loos answered some of the most frequently asked questions about viruses in general, corona viruses, the COVID-19 pandemic, and the future of research in microbiology.
Did you find this helpful? Consider making a donation to the Saskatchewan Science Centre!
Science Says: Wear A Mask
Wearing a mask is a simple thing that you can do to help protect yourself and others from COVID-19. The more things you can do (masking up, social distancing, staying home when possible) the more protection you afford to yourself and those around you, including the people that you love.
This is Part 4 of a series explaining the COVID-19 pandemic. Please consider starting at Part 1: What is a virus or check out the whole series by clicking the button below.
A Brief History of Mask Usage
Today it’s common knowledge that microorganisms such as bacteria and viruses may cause disease in plants and animals (including humans). But a few centuries ago, the causes of infectious diseases and their methods of transmission were not known. Here is a brief summary of how our understanding of disease transmission has evolved and how science proved that something as simple as wearing a mask helps to prevent the spread of disease.
17th Century
Many of the top scientists of the era believed that disease was carried by bad smells or “miasmas”. As a result, their strategy to avoid spreading disease revolved around the avoidance of bad smells.
The first masks appeared during the later waves of the bubonic plague. A French doctor, Charles de Lorme, designed a special suit for physicians treating plague patients. It consisted of a large leather tunic, gloves, boots, a hat, and a mask in the shape of a bird’s beak that contained aromatic herbs.
Even if the doctors of that time did not know the actual cause of disease transmission, this attire played a part in protecting them from the plague. The leather protected them from disease-carrying fleas, the gloves prevented direct contact with patients, and the herbs in the nose had antiseptic properties, thus neutralizing bacteria passing directly from one individual to another.
19th Century
In the mid-19th century, French chemist and microbiologist Louis Pasteur showed that fermentation and putrefaction are caused by organisms in the air. Later in the 19th century, scientists including Pasteur, Lister, and Koch proposed theories that living organisms called germs were responsible for causing and spreading disease.
“Germ theory, in medicine, the theory that certain diseases are caused by the invasion of the body by microorganisms, organisms too small to be seen except through a microscope.”
-Britannica.com
This theory revolutionized the human understanding of infectious diseases and toppled the miasma theory. In 1870 John Tyndall, an Irish physicist, presented a paper to the Royal Institution in London in which he demonstrated that dust in the air could contain germs and disease and that a cotton-wool respirator could filter them out. Applying his research, he developed a much-improved gas mask for firefighters.
“If a physician wishes to hold back from the lungs of his patient, or from his own, the germs by which contagious disease is said to be propagated, he will employ a cotton wool respirator … Such respirators must, I think, come into general use as defense against contagion.”
-John Tyndall, On Haze And Dust
20th Century
During the early 20th century, various types of cloth masks (made of cotton, gauze, and other fabrics) were used in US hospitals to protect healthcare workers from diphtheria and scarlet fever. Wu Lien-teh, a public-health specialist from Malaya, was investigating a pneumonic plague that had broken out in northern China. He developed a mask from layers of gauze enveloped in cotton, with ties so that it could be hung on the ears. This was the prototype from which the masks currently used in medicine today evolved.
During the 1918 Spanish influenza pandemic, masks made of various layers of cotton were widely used by healthcare workers and the general public. Gauze masks were used during the second Manchurian plague epidemic in 1920–1921 and a pneumonic plague epidemic in Los Angeles in 1924; resulting in a decrease of infection rates among healthcare workers.
During the 1930s and 1940s, gauze and cloth masks were used by healthcare workers to protect themselves from tuberculosis. In the middle of the 20th century, after disposable medical masks had been developed, the use of cloth masks decreased; however, cloth mask use is still widespread in many countries in Asia.
Modern Masks And How they Work
How Can Cloth Masks Prevent the Spread of Disease?
When we breathe, talk, cough, sneeze, or sing, we emit droplets across a range of sizes, and these particles may contain viruses. Putting on a cloth mask can trap these droplets and prevent the virus from spreading to other people.
Cloth is a woven material, with threads intersecting each other in a pattern. It’s true that there are gaps between the threads and that these gaps are larger than the width of a single virus. Sometimes people are lead to believe that the virus is able to simply sail through a mask, but this isn’t true.
.Although the size of a single virus is smaller than the size of the gaps between the individual fabric threads of the mask, the size of the droplets that contain viruses could be bigger than these gaps. In addition, even though there are gaps between the threads in cloth, the individual threads are wider than the gaps. In addition, each thread has microfilaments or imperfections that project into the gap, further providing an obstruction. Finally, a good mask has multiple layers (Health Canada recommends masks with 3 layers) for extra protection.
It’s also worth noting that the droplets containing the virus don’t move in a straight line - they move and swirl in the air which makes them aligning with and passing through a tiny hole very unlikely. And, as droplets are not living things they can’t change direction to go around the fibers or move to avoid obstacles in their path.
Don’t be concerned about an individual gap in the weave of a fabric - instead, think of the entire mask with multiple layers and how everything works together to act as a filter.
Source: Center For Disease Control
Source: The Conversation
What Is An ‘N95’ Mask?
An N95 mask is technically a respirator. In order to use the term N95, the mask (respirator) must be certified by NIOSH - the National Institute for Occupational Safety and Health. During the COVID-19 pandemic we have begun to think of them in association with the medical field, but N95 respirators are used as protection in a number of non-medical fields ranging from autobody repair to construction, welding, and more.
The name N95 is actually a description of the capabilities of the respirator. The ‘N’ means that the respirator is not resistant to oil, and the 95 means that they filter 95% of 0.3 micron and larger materials. There are even multiple types of N95 respirators - including those intended specifically for surgical use and those with or without breathing vent holes.
N95 Respirators utilize capture or filtration to remove airborne particles as described below:
The particles that come in direct contact with the fiber cannot pass through the filter
Larger particles have too much inertia and thus can’t follow the airstream as it is diverted around the filter.
Small particles are easily moved and deviated by air molecules, making it likely that they come into contact with a filter fiber.
For the particles that are neither small enough nor large enough to be captured by any of the methods described above, N95 respirators utilize a type of electrical charge. The charge on the fiber filter attracts the oppositely charged particle, stopping all oppositely charged particles from passing through the filter regardless of their size.
In all cases, once a particle comes in contact with a filter fiber, it is removed from the airstream and strongly held by molecular attractive forces. It is very difficult for such particles to be removed once they are collected.
What’s The Point If Masks Are Not 100% Efficient Or If Other People Don’t Wear Masks?
When it comes to viral science, numbers count. It is true that if everyone in a community wears a mask, the probability of infections drops drastically. The studies clearly show that the more people there are wearing masks, the less the disease will spread.
That is because wearing a mask helps not only the wearer from coming in contact with the virus, but also helps prevent an infected person from spreading the virus. In other words, they offer two-way protection: when breathing in and when breathing out.
Avoiding Misinformation And Memes
There is a lot of incorrect and misleading information available on the internet, and sometimes that information is shared by friends or family members; sometimes even people that we trust.
Just because someone shares incorrect information, that doesn’t mean that they are a bad person - it just means that they’ve made a mistake. Unfortunately, it’s not always easy to tell when a piece of information is wrong. The most convincing, and dangerous, forms of misinformation are those that appeal to our “common sense” or that seem logical when first viewed.
For example, look at this meme often seen on Facebook:
Don’t Be Fooled By Misinformation!
At first look, it appears to make sense: why do I need to wear such a complicated mask when using spray paint, but cloth masks with images of Baby Yoda are enough to protect me from COVID-19?
The answer, also explained above, is simply that while the gaps in a cloth mask may be larger than the size of a single SARS-CoV-2 virus, the virus spreads in liquid droplets. A single layer of cloth might not be great against a single virus, but a multi-layer cloth mask, as recommended by Health Canada, has been proven to be effective against droplets containing the SARS-CoV-2 virus.
Other common pieces of misinformation about masks are that face masks can cause other health problems (not true) or that if you wear a mask you don’t need to practice social distancing (you still do).
Sometimes misinformation comes from a misunderstanding of a scientific article, from old information, or a single report or study that might have errors in it. It’s always a good idea to search for multiple reputable sources of information when trying to confirm a piece of information or advice that you hear.
Wearing a mask is a simple thing that you can do to help protect yourself and others from COVID-19. The more things you can do (masking up, social distancing, staying home when possible) the more protection you afford to yourself and those around you, including the people that you love.
How To Choose The Right Mask
Here are a few things to consider when selecting a mask:
Wear a mask that fits snugly on your face
Put on the mask such that it covers both mouth and nose at all times
Choose a mask with two or more layers of breathable fabric
Use only masks without exhalation valves or vents because they may not prevent you from spreading COVID-19
For more details and the latest updates on mask recommendations, please visit:
World Health Organization: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
Center For Disease Control: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html
Did you find this helpful? Consider making a donation to the Saskatchewan Science Centre!
Wash Your Hands
Washing your hands is a key part of preventing the spread of all diseases, including COVID-19. Read on to find out why.
Soap doesn’t (usually) kill germs, but it can break them up and remove them. Washing your hands is a key part of preventing the spread of all diseases, including COVID-19. Read on to find out why.
This article is part of a series to help people understand COVID-19. Click the button below to see all of the articles in the series.
Wash Your Hands
One of the most effective ways we have to prevent the spread of viruses such as SARS-CoV-2 is to properly wash our hands with warm water and soap. By doing so, we remove highly contagious pathogens from our skin, preventing those pathogens from spreading to other surfaces we touch or to other people around us. A pathogen is a micro-organism such as a bacteria or a virus that can cause disease or illness in a host.
According to the Government of Canada, we know that the SARS-CoV-2 virus (and accordingly, COVID-19) spreads:
"from an infected person to others through respiratory droplets and aerosols created when an infected person coughs, sneezes, sings, shouts, or talks. The droplets vary in size from large droplets that fall to the ground rapidly (within seconds or minutes) near the infected person to smaller droplets, sometimes called aerosols, which linger in the air under some circumstances.
The relative infectiousness of droplets of different sizes is not clear. Infectious droplets or aerosols may come into direct contact with the mucous membranes of another person's nose, mouth or eyes, or they may be inhaled into their nose, mouth, airways and lungs. The virus may also spread when a person touches another person (i.e., a handshake) or a surface or an object (also referred to as a fomite) that has the virus on it, and then touches their mouth, nose or eyes with unwashed hands.”
It’s All About The Molecules
Proper handwashing is such an effective tool to prevent the spread of SARS-CoV-2 and other harmful viruses because of how soap molecules work.
Scientists know that the structure of the SARS-CoV-2 virus contains a crown of external spike proteins that attach to our cells in order to reproduce and spread throughout our bodies.
“The spike protein is the major surface protein that it uses to bind to a receptor — another protein that acts like a doorway into a human cell. After the spike protein binds to the human cell receptor, the viral membrane fuses with the human cell membrane, allowing the genome of the virus to enter human cells and begin infection.”
These spikes are the reason that we call viruses such as SARS-CoV-2 coronaviruses - under a microscope these spikes resemble the corona of the sun, which looks similar to a crown. The Latin word for crown is corona, hence coronavirus.
Soap molecules are a type of surfactant. These molecules have two opposite ends: one which is hydrophilic (likes water) and one which is hydrophobic (does not like water, but DOES like lipids - natural oils and fats). Many bacteria and viruses are surrounded by a protective lipid layer. These lipid layers protect the virus from threats and also help it to stick to our skin. In addition, our skin is covered in oils and the virus can easily attach to those oils.
When we use soap and water to wash our hands the hydrophilic end of the soap molecules attaches readily to the water molecules, but the hydrophobic ends want to get away from the water. One of the best ways to do that is by inserting themselves into the lipid layer of the pathogens (in this case, SARS-CoV-2) and to the oils on our skin.
As we continue to scrub our hands with soap (for at least 20 seconds) we build a lather and lift these oils from our skin and encourage the hydrophobic ends of the soap molecules to connect with the pathogen. When we rinse our hands, the viruses and oils are washed away.
In the case of SARS-CoV-2 (the virus that causes COVID-19) and other viruses, soap is also very good at breaking up the non-covalent bonds that hold the virus together - breaking the virus apart into tiny pieces.
When we rinse the soap lather from our hands, the viruses (and pieces of the virus) which are now attached to the soap molecules are removed from our skin. Without soap molecules to bind to the proteins surrounding the virus, handwashing would not be an effective means for preventing the spread of bacteria and viruses. This means that simply running your hands under water without using soap is not effective.
You can explore soap molecules at home with this simple demonstration.
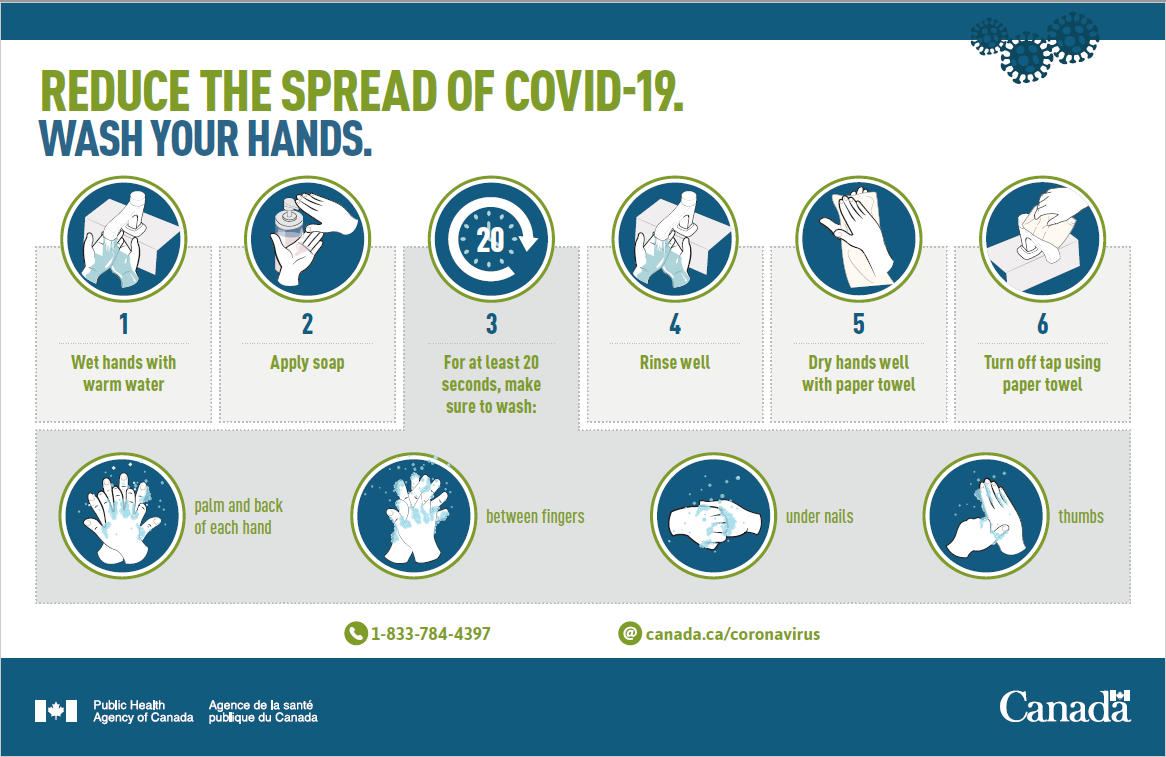
How to Wash Your Hands
Wet your hands with clean, running water.
Apply soap
Lather your hands by rubbing them together: rub your palms together, lather the backs of your hands, between your fingers, under your fingernails, your thumbs and up near your wrists. To make sure your hands are clean lather them for at least 20 seconds (an easy way to keep track of the time is to sing Happy Birthday twice)
Rinse well under clean, running water.
Dry your hands with a paper towel and then use that towel to turn off the tap and open the bathroom door if needed. This ensures your hands remain clean without coming into contact with a potentially contaminated surface like a tap or door handle.
Proper handwashing does more than prevent the spread of COVID-19. According to the Center for Disease Control about 1.8 million children under the age of 5 die each year from diarrheal diseases and pneumonia. It is estimated that handwashing alone could protect 1/3rd of these kids from diarrhea and 1/5th of these kids from pneumonia.
Some Additional Notes That May Be Helpful:
Because the temperature of the water is never hot enough to kill pathogens, even cold water can be used to wash your hands. Some health organizations do state to use warm water, however. This is because warm water may help to maximize the lathering effect of soap.
Drying your hands with a clean towel may improve the benefits of handwashing - the towel can help to remove additional pathogens that may not have rinsed off during the handwashing process.
Running water is a key component to rinse away the germs. Don’t simply use a still tub of water. Remember, handwashing doesn’t kill the germs - it lifts them from your skin and allows you to rinse them away.
Global Handwashing Day is celebrated annually on October 15.
What About Hand Sanitizer?
Hand sanitizer is an alcohol-based chemical compound that has been proven to kill many bacteria and viruses. Hand sanitizer, as long as it contains at least 60% alcohol, is effective in helping prevent the spread of harmful pathogens when access to clean, warm water and soap is not available. One of the key steps in using hand sanitizer is to ensure that it dries on the skin - do not rinse or wipe off hand sanitizer before it is dry or the effectiveness will be compromised.
However, the best option is always to wash your hands with soap and clean running water. Proper handwashing removes all types of germs from your skin, preventing spread and infection, while hand sanitizer works by killing certain germs on the skin. Handwashing can also remove chemicals such as pesticides and certain heavy metals from your skin, and will remove germs that hand sanitizer can not. As a result, alcohol-based hand sanitizers should be used if soap and water are not available, not as an alternative to washing your hands with soap and water.
Additional Sources And Reading
Government of Canada: Coronavirus disease (COVID-19): Prevention and risks
Government of Saskatchewan: COVID-19
World Health Organization: Coronavirus disease (COVID-19) pandemic
Did you find this helpful? Consider making a donation to the Saskatchewan Science Centre!